Notes in the Margin - 24 September 2024
MAID and Palliative Care, Delirium, EMR Use in the Clinic, and More
Notes from a Family Meeting is a newsletter where I hope to join the curious conversations that hang about the intersections of health and the human condition. Poems and medical journals alike will join us in our explorations. If you want to come along with me, subscribe and every new edition of the newsletter goes directly to your inbox.
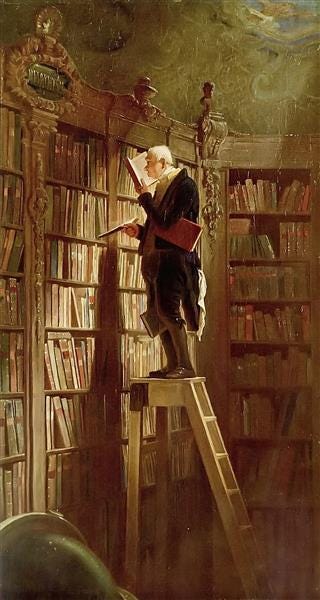
Every so often, I’ll share things I’ve been reading with a few words of mine scribbled in the margins. If you have something to share, please do! The comment section is open.
“Rehabbed to Death” in Oncology: Where Do We Go From Here?
A mysterious question I encounter in my work is whether someone with advanced cancer will benefit from short-term rehabilitation in pursuit of the goal to live longer. To facilitate that goal, they need to get stronger to endure the rigors of cancer-directed therapy. One remarkable challenge these authors highlight, in addition to those you might expect, is the reverence clinicians have for the relationship oncologists have with their patients. This relationship might inhibit helpful goals of care conversations. We’ve still got a long way to go…
Is medical assistance in dying part of palliative care?
Using a framework recently published in the Journal of the American Geriatrics Society, Harvey Chochinov and Joseph Fins determine that “medical assistance in dying” (the euphemism that encompasses both assisted suicide and euthanasia [ASE]) falls outside the scope of medicine. Their argument is subtle in that they don’t argue that ASE is immoral in and of itself nor that ASE should be illegal, but merely that it isn’t medical care and therefore can’t fall within the purview of palliative care. Neither do they draw out the implications of their argument, though anyone who is sympathetic to it probably doesn’t find ASE too appealing in any context.
Drugs, Delirium, and Ethics at the End of Life
Columba Thomas and colleagues write carefully about using medications well to manage delirium at the end of life. It’s not so easy to just hammer someone with the highest possible dose of medication. They make this argument in part by relying on Dan Sulmasy’s previously argued canons of therapy (about which I write here).
National Comparison of Ambulatory Physician Electronic Health Record Use Across Specialties
Some studies present evidence that you knew was there, but it’s still a gut-punch to see. Outpatient clinicians are spending enormous amounts of time interacting with their computers, time after work and even on days they’re not scheduled to work. It should come as no surprise that a specialty like infectious disease has the highest documentation burden while anesthesiology has the lowest. This almost certainly influences career choice for those graduating from medical school.
Medical Humanities and the Specialist
Ronald Dworkin argues that without the medical humanities, the medical specialist is hobbled and prideful. They have no appreciation for their limits. They struggle to think, which is dangerous because medicine is more than science. However, Dworkin’s utilitarian bent during the essay sets the humanities up to be co-opted for medicine’s agenda. Clinicians need the humanities to do the work clinicians do. I would argue that, first, people need the humanities to become the kinds of people they need to become, and that includes medical specialists.
From the Archives
Here's something, only a little dusty, that new readers may not have seen.
Something I never learned a lot about in medical school was health. Sure, I learned about anatomy and physiology, I learned about disease and therapy, but there weren’t any lectures on what it means for someone to be healthy. It seems obvious, but its obviousness is what sometimes makes it so elusive.
What is Health?
I sat on my porch one day, drinking tea and reading. My daughter played in the driveway, spinning in her dress and drawing with chalk on the cement. A light breeze played through the leaves above us, bringing the first cool promises of autumn amidst the summer’s heat. Her effortless movements, a blessing as much for me in that moment as for her, reminde…